Insurance carriers can sometimes be set up in error. This can happen when you accidentally add a carrier that already exists in your database, or you enter a carrier with an unsupported Payer ID 06126, thinking it was the supported version of a carrier. In either situation, you can fix these errors using the merge carrier feature in Dentrix Ascend. Merging carriers is the act of combining two carrier records into one master carrier record.
Watch this video to learn how to merge insurance carriers. (Duration: 3:08)
Created February 2023
Additional Information
- Once you merge two insurance carriers, the action cannot be undone.
- To merge insurance carriers, you must have the Merge Carriers right assigned to your user role.
- When you merge a carrier from a 06126 status to a recognized carrier, you can:
- Perform automated eligibility verification for patients with that carrier.
- Send attachments with claims.
- Send claims electronically for a faster turn-around.
- When you merge carriers, the original plan information remains the same.
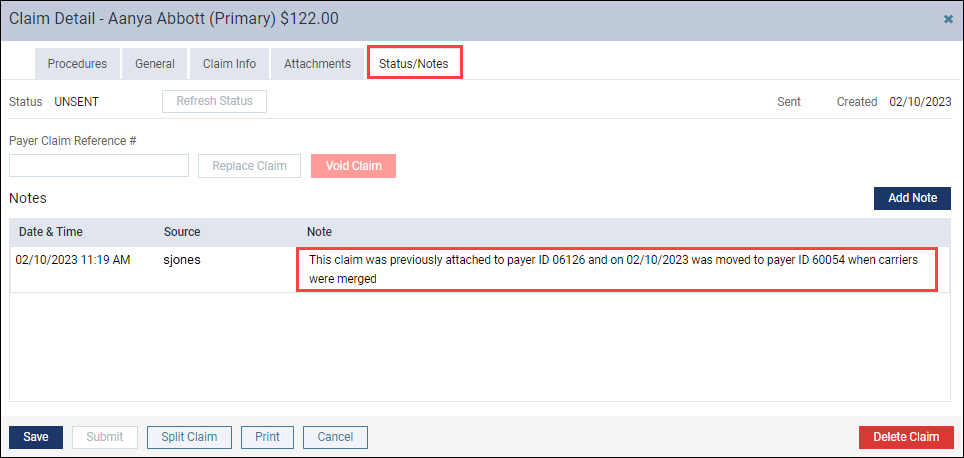
- After you merge carriers, a note is added to the Claim Detail on the Status/Notes tab. The note confirms the old Payer ID number that the claim was attached to, the date the claim was moved, and the new Payer ID number to help you track the history of the claim.