The product update released January 20, 2022, introduces enhancements related to insurance coordination and insurance claims. Power Reporting has a couple of new fields.
Insurance
New Workflow for Switching Primary and Secondary Insurances
The previous release introduced an easier workflow for switching primary and secondary insurance plans. This release includes additional enhancements to that workflow:
- Swapping insurance coordination order using drag and drop
- Handling unsent claims with credit adjustments
Note: For more information on how to deal with outstanding claims attached to insurance plans or how to review the history of insurance coordination order changes, review the 385 Release Notes.
Swapping Insurance Coordination Order Using Drag and Drop
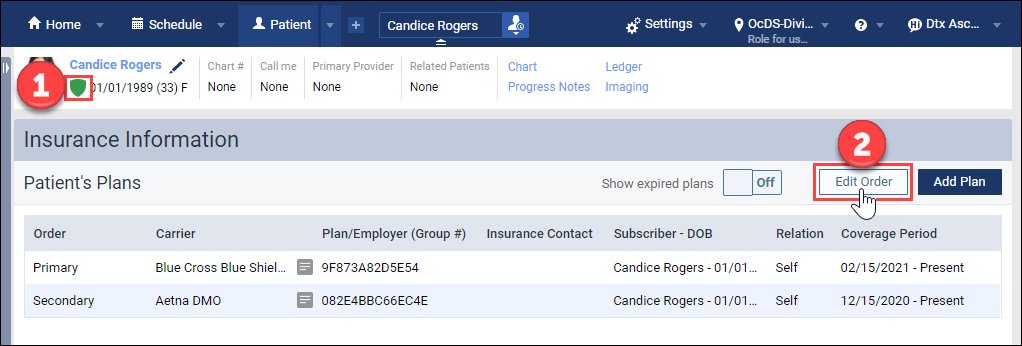
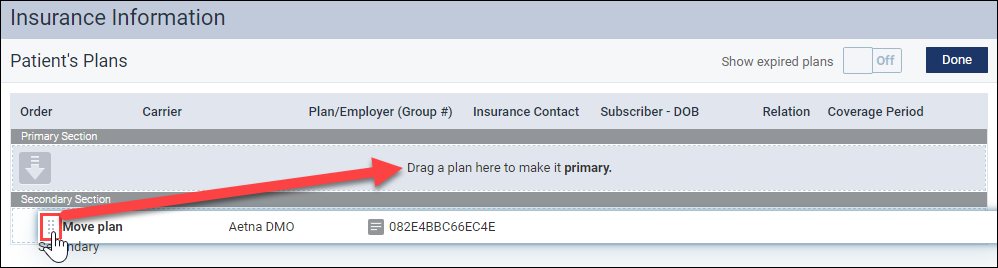
In the patient information ribbon, click the green shield icon to see a patient’s insurance information. On the Insurance Information page, click Edit Order.
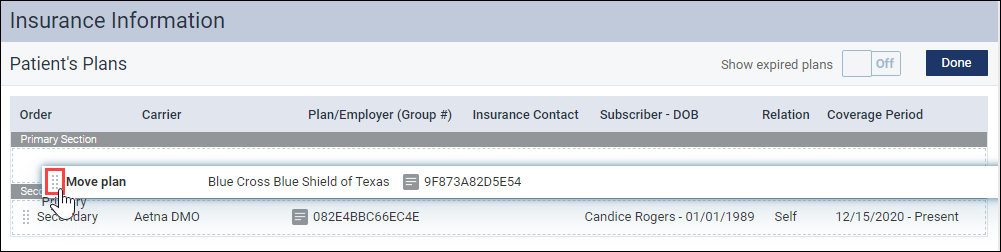
Select the grab-handle icon next to the plan you would like to move. Then drag and drop the plan to the desired position.
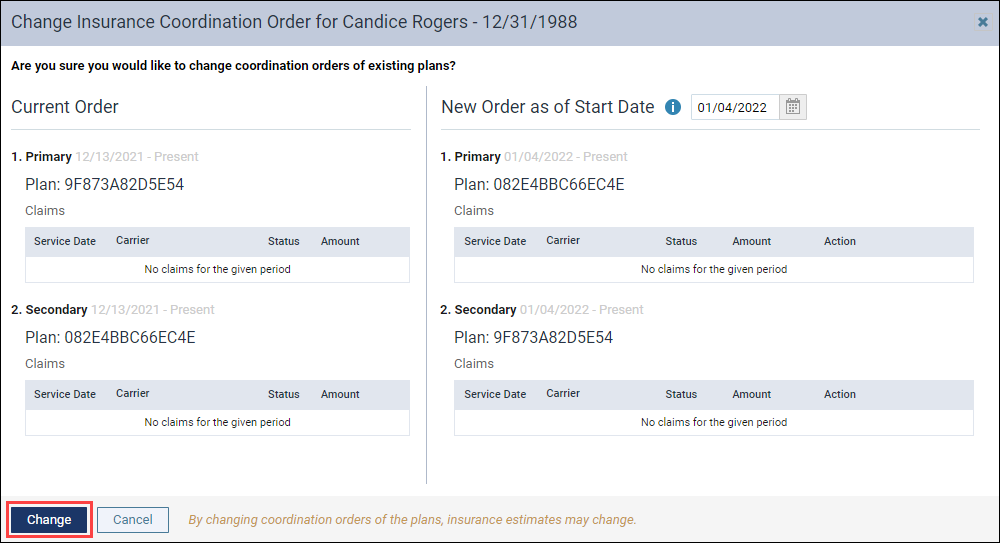
When you move an insurance plan, the Change Insurance Coordination Order dialog appears. You see the current state of the insurance plans on the left and the desired state on the right. Click Change to confirm the new order of insurance plans.
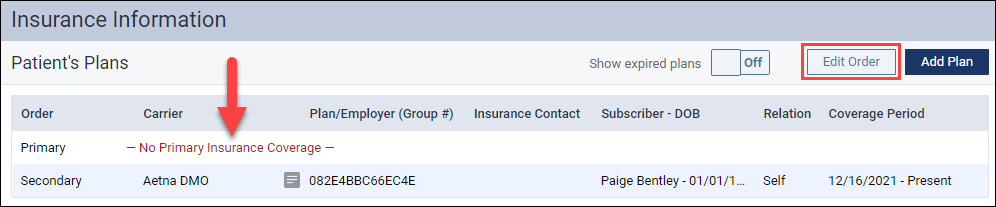
The new order is reflected on the Insurance Information page.
The Edit Order functionality can also be used when the primary insurance has expired, and you would like to promote the secondary insurance to the primary insurance.
Handling unsent claims with credit adjustments
Sometimes when you are trying to switch the primary and secondary insurances, Dentrix Ascend will warn you that you have unsent claims with credit adjustments in a closed period. You must delete these credit adjustments before proceeding with the insurance order change. To do this, click View credit adjustment.
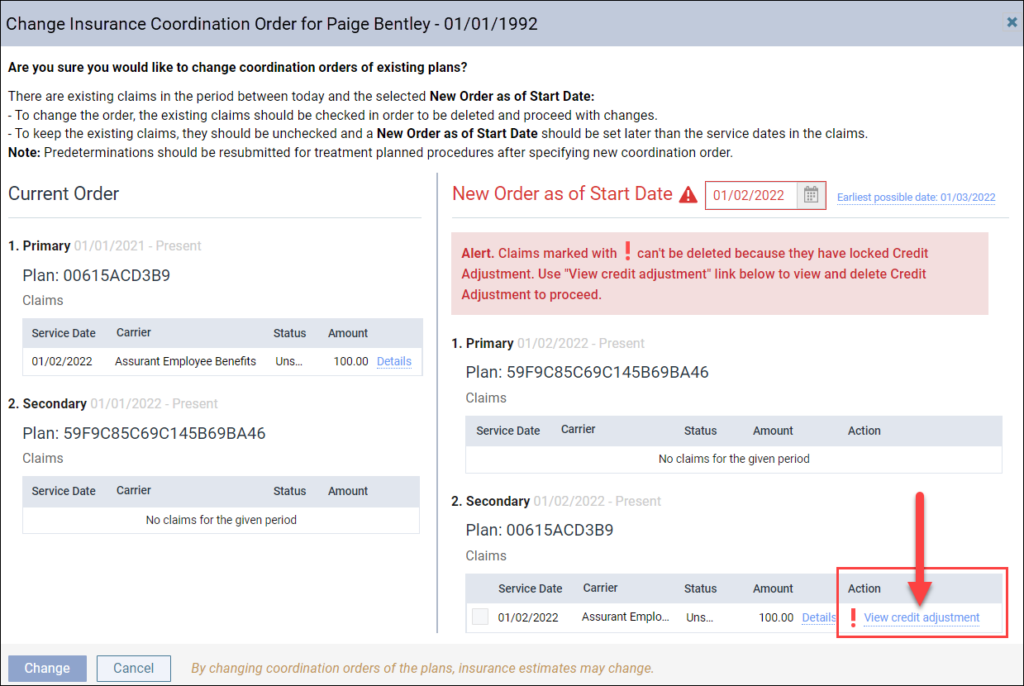
When you click View credit adjustment, the View Credit Adjustment dialog appears. An authorized user must click the lock icon in the upper-right corner and enter their credentials to unlock the credit .


Once the credit adjustment is unlocked, close the Edit Credit Adjustment . You do not need to click Save. The credit adjustment will now be deleted along with the unsent claim. You are now able to click Change and proceed with the insurance order change.

Refresh Claim Status
A new enhancement has been added to the Claim Detail dialog box. You can now manually request an update from the clearinghouse for the claim if the automatic update between Dentrix Ascend and the clearinghouse was interrupted. When you click the new Refresh Status button, Dentrix Ascend refreshes the claim with the most recent status that the clearinghouse has received from the carrier.
To use this new enhancement, open a submitted claim and then select the Status/Notes tab. You will see a new Refresh Status button.
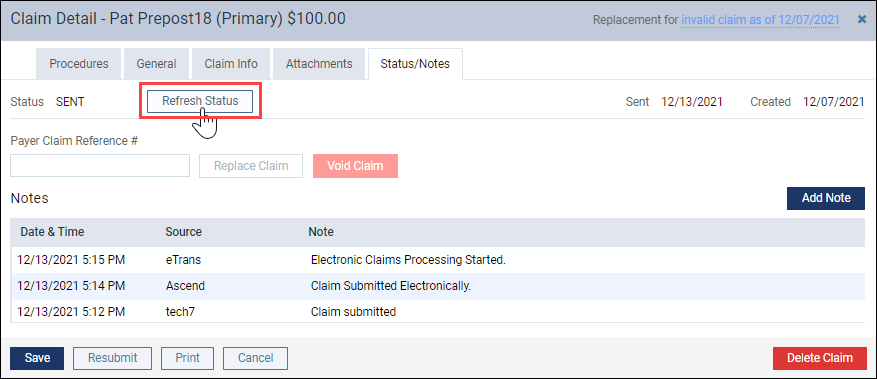
The button is active when there has been no status update received from the clearinghouse in the last two days. When you click Refresh Status, Dentrix Ascend immediately updates the status of the claim with the information that the clearinghouse has. If the status has changed, the new status appears next to the Status field. Also, under the Notes section, Ascend adds a note that the claim status was refreshed.

Note: The Refresh Status button becomes active after two days from the clearinghouse. Once you click this button, it becomes inactive. After two days, the button may become active again, and you can request another update if you wish. This should not, however, be necessary under normal circumstances.
Set Predetermination Requirements – Feature Update
This feature is still under construction. When completed, it will save time and remind team members to send out predeterminations when needed. This update includes new additions to the new Manage Predeterminations window. This is where you will be able to select which procedures require predetermination.
To see the Manage Predeterminations window, open an insurance plan and click the new Predeterminations button.

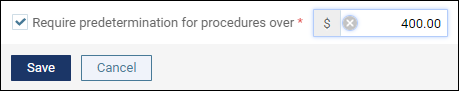
The Manage Predeterminations window is where you will select the procedures in this specific plan that require predeterminations. Note that the entire organization will share the plan settings. New in this window are the Replace with search box, and the Require predetermination for procedures over field.
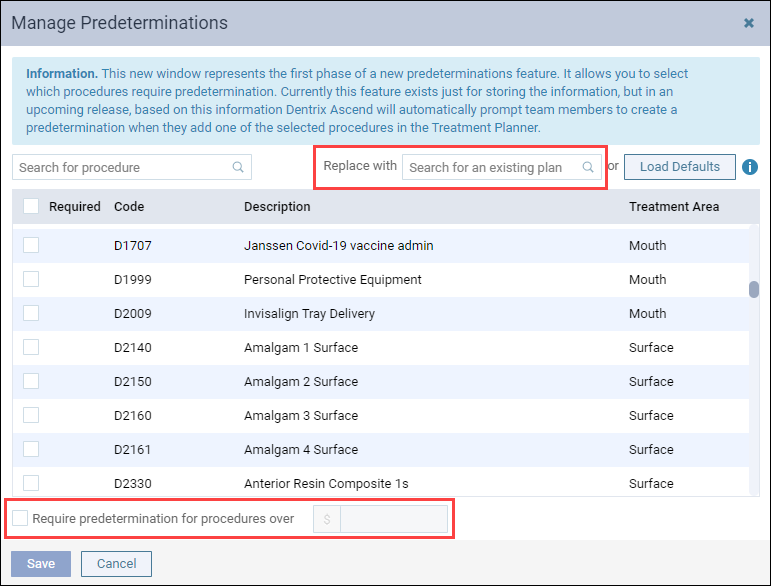
The Replace with search box will allow you to find another insurance plan for which you have already done the work of configuring and import the selections to this plan. This can be a great time saver. As with the Load Defaults option, you will be instructing Dentrix Ascend to replace any existing selections. The best workflow is to import the defaults or the configuration of another plan and then make your adjustments.

The Require predetermination for procedures over field, when it gets implemented, will allow you to set predetermination requirements based on a financial threshold, as directed by the carrier. Check the box, and enter a dollar amount. All procedures whose fee exceeds that amount will automatically be marked as requiring a predetermination. Like the other tools in this window, applying a financial threshold will wipe out any configuration you may have already done.
Power Reporting
New Fields Supporting Insurance Coordination Changes
As an adjunct to the updates that now allow you to switch primary and secondary insurance plans more easily, the Analysis Patient Insurance Report Builder has two new fields in the Insurance category. The fields, Resp. Order End Date and Resp. Order Start Date, refer to the dates upon which an insurance plan, respectively, stopped and started being responsible as the primary, secondary, tertiary, or other plan for a given patient. Naturally, an active plan without a current end date will return a value of Not Available for the end date.

Do not be confused by what may appear to be two primary insurance plans on the same day. When you switch plans on the same day, one was and one now is the primary. The date field is just a date and does not include a timestamp to show you when the switch occurred.
No default reports currently make use of these new fields.
User Rights
No new user rights were introduced in this release.
New Learning Content
As the Dentrix Ascend software continues to change and improve, the Practice Success library also expands and updates when needed. Click a title below for some great new content.
Entering an Electronic Patient Prescription
Sending an electronic prescription is convenient for your patients and helps your practice avoid mistakes, delays, and safety risks associated with written prescriptions. Watch this step-by-step tutorial to learn how to enter an electronic patient prescription.
Print & Mail for Me
Sending billing statements to patients is time consuming and expensive, and it requires the office to maintain an inventory of supplies. Print & Mail for Me is an integrated print statement fulfillment option that allows you to send paper billing statements directly from Dentrix Ascend to the patients of your choice.
