EARLY ACCESS ONLY
Previously, you could validate the subscriber ID for only primary insurance plans. Now, you can validate the subscriber ID for secondary, tertiary, and quaternary insurance plans.
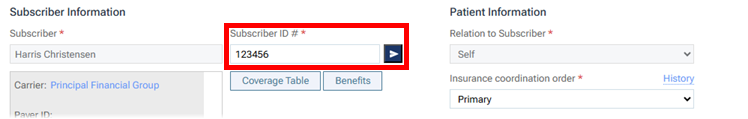
To validate a subscriber ID
- Do one of the following:
- If you are adding a patient’s primary insurance plan, specify at least the following information: Subscriber; Carrier, Payer ID, and Plan; and Subscriber ID #.
- If you are editing a patient’s primary insurance plan, change the Subscriber ID # if necessary.
- If you are adding a patient’s primary insurance plan, specify at least the following information: Subscriber; Carrier, Payer ID, and Plan; and Subscriber ID #.
- Click the Check Subscriber ID button
 next to the Subscriber ID # box.
next to the Subscriber ID # box.
Notes: The following still applies to the validation process:
- This validation process is supported only if the payer supports standard data (Eligibility Essentials) requests. Even if the payer supports enhanced data (Eligibility Pro) requests, if it does not support standard data (Eligibility Essentials) requests, the validation will fail and display a “Payer ID Not Supported” error.
- This validation process does not provide a breakdown of the patient’s eligibility for coverage. A .pdf file with eligibility details is not saved to the patient’s Document Manager, and an option to import insurance details is not available. Those eligibility details are available only for eligibility verifications that are performed for scheduled appointments (see the topics about verifying eligibility statuses and importing insurance information).
